Child Behavioral Issues
All young children can be naughty, defiant and impulsive from time to time, which is perfectly normal. However, some children have extremely difficult and challenging behaviours that are outside the norm for their age.
The most common disruptive behaviour disorders include oppositional defiant disorder (ODD), conduct disorder (CD) and attention deficit hyperactivity disorder (ADHD). These three behavioural disorders share some common symptoms, so diagnosis can be difficult and time consuming. A child or adolescent may have two disorders at the same time. Other exacerbating factors can include emotional problems, mood disorders, family difficulties and substance abuse.
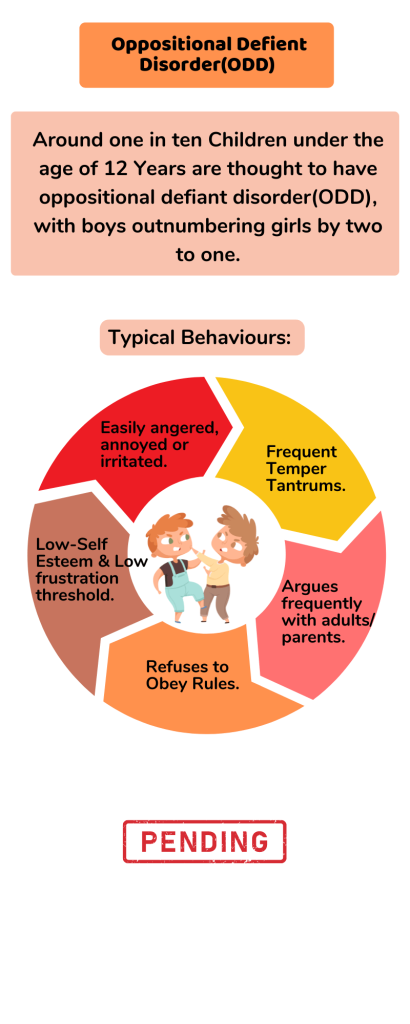
Oppositional defiant disorder
Around one in ten children under the age of 12 years are thought to have oppositional defiant disorder (ODD), with boys outnumbering girls by two to one. Some of the typical behaviours of a child with ODD include:
- Easily angered, annoyed or irritated
- Frequent temper tantrums
- Argues frequently with adults, particularly the most familiar adults in their lives, such as parents
- Refuses to obey rules
- Seems to deliberately try to annoy or aggravate others
- Low self-esteem
- Low frustration threshold
- Seeks to blame others for any misfortunes or misdeeds.
Conduct disorder
Children with conduct disorder (CD) are often judged as ‘bad kids’ because of their delinquent behaviour and refusal to accept rules. Around five per cent of 10 year olds are thought to have CD, with boys outnumbering girls by four to one. Around one-third of children with CD also have attention deficit hyperactivity disorder (ADHD). Some of the typical behaviours of a child with CD may include:
- Frequent refusal to obey parents or other authority figures
- Repeated truancy
- Tendency to use drugs, including cigarettes and alcohol, at a very early age
- Lack of empathy for others
- Being aggressive to animals and other people or showing sadistic behaviours including bullying and physical or sexual abuse
- Keenness to start physical fights
- Using weapons in physical fights
- Frequent lying
- Criminal behaviour such as stealing, deliberately lighting fires, breaking into houses and vandalism
- A tendency to run away from home
- Suicidal tendencies – although these are more rare.

Attention deficit hyperactivity disorder
Around two to five per cent of children are thought to have attention deficit hyperactivity disorder (ADHD), with boys outnumbering girls by three to one. The characteristics of ADHD can include:
- Inattention – difficulty concentrating, forgetting instructions, moving from one task to another without completing anything.
- Impulsivity – talking over the top of others, having a ‘short fuse’, being accident-prone.
- Over activity – constant restlessness and fidgeting.
Risk factors in children’s behavioural disorders
The causes of ODD, CD and ADHD are unknown but some of the risk factors include:
- Gender – boys are much more likely than girls to suffer from behavioural disorders. It is unclear if the cause is genetic or linked to socialisation experiences.
- Gestation and birth – difficult pregnancies, premature birth and low birth weight may contribute in some cases to the child’s problem behaviour later in life.
- Temperament – children who are difficult to manage, temperamental or aggressive from an early age are more likely to develop behavioural disorders later in life.
- Family life – behavioural disorders are more likely in dysfunctional families. For example, a child is at increased risk in families where domestic violence, poverty, poor parenting skills or substance abuse are a problem.
- Learning difficulties –problems with reading and writing are often associated with behaviour problems.
- Intellectual disabilities – children with intellectual disabilities are twice as likely to have behavioural disorders.
- Brain development – studies have shown that areas of the brain that control attention appear to be less active in children with ADHD.
Where to get help
- Paediatrician
- Child psychologist
- Child psychiatrist
Treatment of behavioural disorders in children
Untreated children with behavioural disorders may grow up to be dysfunctional adults. Generally, the earlier the intervention, the better the outcome is likely to be. Research studies indicate that medication management and behavioural treatment for ADHD improved all measures of behaviour in school and at home. Treatment is usually multifaceted and depends on the particular disorder and factors contributing to it, but may include:
- Parental education – for example, teaching parents how to communicate with and manage their children.
- Family therapy – the entire family is helped to improve communication and problem-solving skills.
- Cognitive behavioural therapy – to help the child to control their thoughts and behaviour.
- Social skills training – the child is taught important social skills, such as how to have a conversation or play cooperatively with others.
- Anger management – the child is taught how to recognise the signs of their growing frustration and given a range of coping skills designed to defuse their anger and aggressive behaviour. Relaxation techniques and stress management skills are also taught.
- Support for associated problems – for example, a child with a learning difficulty will benefit from professional support.
- Encouragement – many children with behavioural disorders experience repeated failures at school and in their interactions with others. Encouraging the child to excel in their particular talents (such as sport) can help to build self-esteem.
- Medication – to help control impulsive behaviours.
EATING DISORDERS AND THEIR IMPACT
Eating Disorders are mental health conditions associated with Cravings, Obsessions, and Perceptions. These disorders are much more complex than eating behaviours and have both psychological and physiological consequences. ICD-10(International Classification of Diseases) specifically describes two syndromes namely, Anorexia Nervosa and Bulimia Nervosa and mentions other eating disorders such as Obesity and Pica. Causes of these disorders can be biological or sociocultural influences. jk Anorexia Nervosa: It is associated with self-induced weight loss. Generally, adolescent girls, young women exhibit this disorder. X is a 13-year-old girl. She was tall and healthy girl in the class till she was 12. At 12, due to socio-cultural factor, she perceived herself as fat and developed a cognitive distortion that a girl should be lean to look good and wear slim fits. She then developed Body-Image Distortion. There was constant fear of increase in the weight. Hence, she started Restricted diet and avoided fats. She indulged in excessive exercising. Very soon her weight reduced drastically. From then, her weight was below than expected of her age and height. She lost her appetite(self-induced) and developed Insomnia. Gradually, she developed low self-esteem and started avoiding playing with her friends (social withdrawal). Menstruation cycle got disturbed. Bulimia Nervosa: Here, individual exhibits repeated bouts of overeating and induced vomiting or purging. Generally, it is observed in adolescent girl and young women. Y, 18-year-old female is obsessed with flat tummy (socio-cultural factor). She is preoccupied with eating. On the other extreme, she also has irresistible craving for fast food. She would starve for 5 days in a week. During weekends, her craving overpowers her, and she eats all kinds of fast food. To counteract fattening effect, she resorts to self-induced vomiting. She develops constant fear of fat tummy and constantly checks her structure in the mirror. Whenever she feels she has crossed her threshold weight, she resorts to vomiting. If she meets someone who is thinner than her (according to her), she used to have low moods for days. Pica: Pica is eating non-food materials such as chalk, mud, sand, slate pencils, soap etc. Generally, it is observed in kids, pregnant women who crave for non-food stuff because of hormonal imbalances. Here is an instance of a 48-year-old female who had the habit of eating slate pencils during childhood, and she would regress to the habit whenever she felt negative emotions. She started eating slate pencils at the age of 13 while doing her domestic chores as eating slate pencils made her work easy. She stopped after few years. Her cravings increased during her second pregnancy, and she stopped post-delivery. Iron deficiency was noticed in her blood reports. Later in her married life to deal with stress, she again started eating slate pencils. Slowly she complained of constipation and gradually it led to Piles. Her anxiety led to IBS (irritable bowel syndrome). Eating slate pencils became a vicious circle!! Conclusion: Generally, Eating Disorders can be observed by the caregivers in case of Pica, and by the family members or friends in case of other eating disorders. When such behaviours are noticed, seeking the help of Mental Health Professional immediately helps patient to recover and prevent further recurrence. Seeking Mental Health assistance requires one step out of stigma threshold.
– Manjula Gudapati
Down syndrome
I met Prashant (name changed) a cute, smiling and adorable 5year old kid in 2009 when I was working in a special school. He was unable to speak, read or write which his peers could at 5years.He was very expressive with gestures and actions. He was so special, unique and different. What was it that made him unique? Prashant was born with Down Syndrome.
Down syndrome is a genetic disorder in which there is an extra full or partial chromosome 21. For most people with Down syndrome, this anomaly causes a host of distinctive physical characteristics as well as potential intellectual, health and medical problems
The first indication a child might have Down syndrome can appear during routine prenatal testing. On an ultrasound (an image of a developing fetus, also called a sonogram), visible signs a baby may have Down syndrome include:
- Excess skin in the back of the neck
- A shorter-than-normal femur (thigh) bone
- A missing nose bone
People with Down syndrome share a host of recognizable facial and physical feature. The obvious characteristics of Down syndrome include:
- A round face with a flat profile and small nose and mouth
- A large tongue that may protrude from the mouth
- Almond-shaped eyes with skin that covers the inner eye
- White flecks in the colored part of the eyes
- Small ears
- A small head that’s somewhat flat in the back
- Short neck
- A single crease across the palm of each hand, short stubby fingers, and a pinkie finger that curves inward
- Small feet with a larger than normal space between the big and second toes
- Short, stocky build
Prashant greatly benefited from occupational therapy, speech therapy and special education. Most differently abled children have unique talents which the parents, school, professionals and community should encourage. I have seen talented musicians, dancers and gymnasts who excelled in spite of being born with this condition.
Low muscle tone: Infants with Down syndrome often appear “floppy” due to a condition called hypotonia.
Sleep
Sleep is very basic biological need of every species. It is the only way for us to relax and stay healthy. Individuals above 20 years age needs approximately 6 to 8 hours of sleep every day.
Sleep is disturbed due to various physical and emotional disturbances. In the present times the number of insomnia cases are increasing due to changes in life-style, diet habits, odd working hours, rotations in job shifts, chatting and browsing on internet, internet gaming, watching movies and web series, hanging out with friends till late nights. These factors disturb the biological clock and circadian rhythm which timely releases sleep hormones put us to sleep naturally.
It is estimated that 6.4% of healthy individual suffer insomnia or poor quality of sleep. This count increases to 83.4% among people who suffer with emotional disturbances and psychiatric illnesses.
A person with poor quality of sleep tends to may suffer with one or many of these problems:
- Remain dull and inactive during the day
- Attention and concentration levels reduce
- Faces Memory disturbances and forgetful
- Difficulty in decision making
- Suffer anxiety or depression in the long run.
- Becomes increasingly irritable.
- Immune system suppresses.
Practice Sleep Hygiene
Do’s
- Maintain a regular sleep wake cycle by going to bed and waking up on the same time every day.
- Exercise regularly.
- Spend some time under sun light every day.
- Keep your bed room free from external noises and lights.
- Warm water bath in the evening.
Don’ts
- Don’t sleep for long hours during the day – a 10 to 15 minutes of power nap is ok.
- Don’t thinking about unresolved problems when you go to bed.
- Don’t watch TV, read books, or work on laptop in the bed
- Don’t consume Tea, Coffee, Coke, and Cigarettes after evening.
- Avoid Alcohol.
Good quality of sleep is very essential for us to stay healthy physically and emotionally. If required take therapist help if you are finding difficult to deal yourself.